Intro
Unlock the secrets of Central Venous Pressure (CVP) range and its crucial role in patient care. Learn how to interpret CVP readings, understand normal and abnormal ranges, and discover the significance of variations in CVP values. Get insights into the diagnostic and monitoring applications of CVP in ICU and clinical settings.
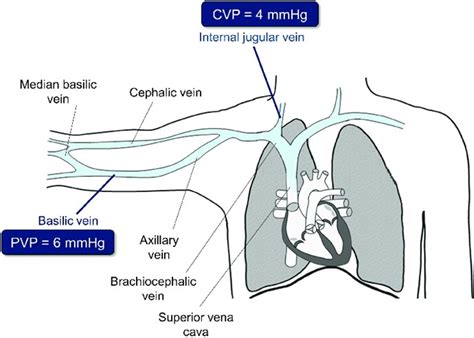
Central venous pressure (CVP) is a crucial measure of the pressure within the superior and inferior vena cava, which are the two major veins that return deoxygenated blood to the heart. Understanding CVP range is essential for healthcare professionals, as it provides valuable information about a patient's cardiovascular and respiratory status. In this article, we will delve into the world of CVP, exploring its importance, normal range, and factors that affect it.
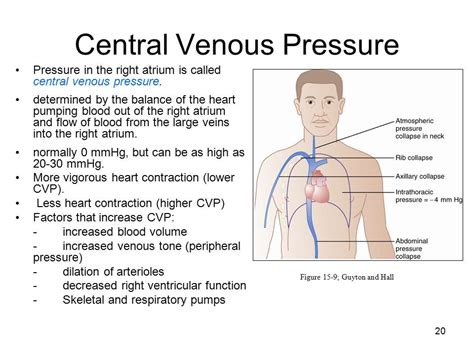
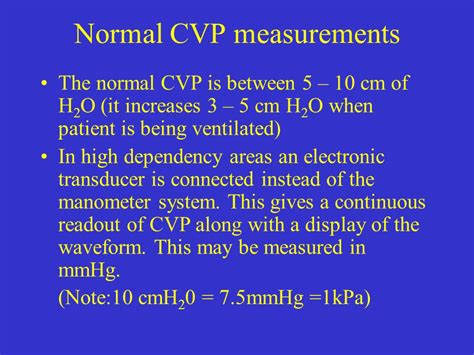
CVP is measured in millimeters of mercury (mmHg) and is typically obtained through the insertion of a central venous catheter into the superior vena cava. The normal CVP range is between 6-12 mmHg, with some sources citing a range of 4-14 mmHg. However, it's essential to note that CVP can vary depending on several factors, such as the patient's position, respiratory rate, and cardiac output.
CVP Range Interpretation
Interpreting CVP range requires a comprehensive understanding of the underlying physiology. A CVP within the normal range indicates that the patient's cardiovascular system is functioning correctly, with adequate blood return to the heart. However, deviations from the normal range can signal potential problems.
Elevated CVP (>12 mmHg) can be caused by various factors, including:
- Cardiac tamponade
- Pulmonary hypertension
- Right ventricular failure
- Volume overload
- Increased intrathoracic pressure
On the other hand, low CVP (<6 mmHg) can be indicative of:
- Hypovolemia
- Cardiac dysfunction
- Decreased intrathoracic pressure
- Increased venous capacitance
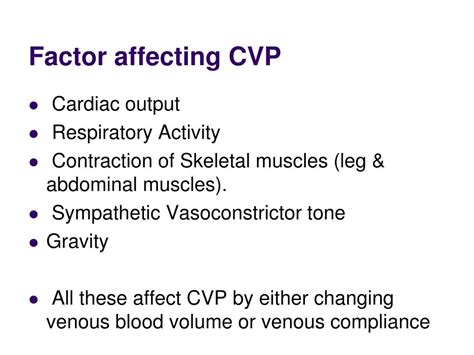
Factors Affecting CVP
Several factors can influence CVP, including:
-
Position
CVP can vary depending on the patient's position. For example, CVP tends to be higher when the patient is in the supine position and lower when in the upright position. -
Respiratory Rate
Changes in respiratory rate can affect CVP. For instance, rapid breathing can decrease CVP, while slow breathing can increase it. -
Cardiac Output
Cardiac output has a direct impact on CVP. Increased cardiac output can lead to elevated CVP, while decreased cardiac output can result in low CVP. -
Volume Status
CVP can be influenced by the patient's volume status. Volume overload can cause elevated CVP, while hypovolemia can lead to low CVP.
Clinical Applications of CVP
CVP has numerous clinical applications, including:
-
Fluid Management
CVP can guide fluid management in critically ill patients. For example, a low CVP may indicate the need for fluid administration, while an elevated CVP may suggest fluid restriction. -
Cardiac Function Assessment
CVP can provide valuable information about cardiac function. Elevated CVP can be indicative of right ventricular failure, while low CVP may suggest cardiac dysfunction. -
Respiratory Monitoring
CVP can be used to monitor respiratory function. Changes in CVP can indicate alterations in intrathoracic pressure, which can be useful in patients with respiratory failure.
Limitations of CVP
While CVP is a valuable tool in clinical practice, it has several limitations. These include:
-
Operator Dependence
CVP measurement can be operator-dependent, and incorrect placement of the central venous catheter can lead to inaccurate readings. -
Lack of Standardization
There is a lack of standardization in CVP measurement, which can make it difficult to compare values across different institutions. -
Interpretation Challenges
Interpreting CVP can be challenging, especially in patients with complex cardiovascular and respiratory conditions.
Conclusion
In conclusion, understanding CVP range is essential for healthcare professionals, as it provides valuable information about a patient's cardiovascular and respiratory status. While CVP has several limitations, it remains a valuable tool in clinical practice, guiding fluid management, cardiac function assessment, and respiratory monitoring.
We invite you to share your thoughts and experiences with CVP in the comments section below. How do you use CVP in your clinical practice? What challenges have you faced in interpreting CVP values?
What is the normal range of CVP?
+The normal range of CVP is between 6-12 mmHg.
What are the factors that affect CVP?
+Factors that affect CVP include position, respiratory rate, cardiac output, and volume status.
What are the clinical applications of CVP?
+CVP has several clinical applications, including fluid management, cardiac function assessment, and respiratory monitoring.
