Intro
Unlock the potential of remote work in healthcare with Remote Utilization Review Nurse Jobs. Discover the growing demand for UR nurses, their roles, and responsibilities. Learn how to leverage your nursing skills for a fulfilling career in utilization review, case management, and healthcare consulting from the comfort of your own home.
The healthcare industry is undergoing a significant transformation, driven by the need for cost-effective and high-quality patient care. One of the key factors contributing to this shift is the increasing demand for remote utilization review nurse jobs. As the healthcare landscape continues to evolve, the role of utilization review nurses is becoming more crucial than ever. In this article, we will delve into the world of remote utilization review nurse jobs, exploring the benefits, requirements, and opportunities available in this field.

What is Utilization Review Nursing?
Utilization review nursing is a specialized field that involves evaluating the medical necessity and appropriateness of healthcare services, treatments, and procedures. Utilization review nurses work with healthcare providers, patients, and insurance companies to ensure that patients receive high-quality, cost-effective care. Their primary goal is to optimize patient outcomes while minimizing unnecessary healthcare expenditures.
Key Responsibilities of Utilization Review Nurses
The responsibilities of utilization review nurses can vary depending on the specific job and employer. However, some common tasks include:
- Conducting medical record reviews to assess the necessity and effectiveness of treatments and services
- Collaborating with healthcare providers to develop treatment plans and ensure compliance with medical policies
- Communicating with patients and families to educate them on treatment options and healthcare benefits
- Analyzing data and trends to identify opportunities for quality improvement and cost reduction
- Developing and implementing utilization management policies and procedures
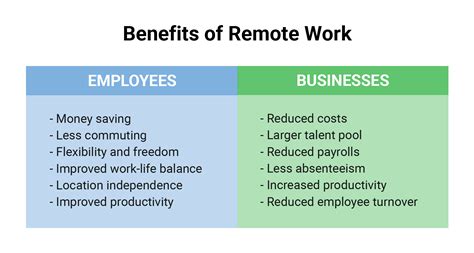
Benefits of Remote Utilization Review Nurse Jobs
Remote utilization review nurse jobs offer a range of benefits for nurses, including:
- Flexibility and autonomy: Remote work arrangements allow nurses to work from anywhere, at any time, as long as they have a stable internet connection.
- Improved work-life balance: Without the need to commute, nurses can spend more time with family and friends, pursue hobbies, or focus on self-care.
- Increased job opportunities: Remote work expands job opportunities, allowing nurses to work with employers across the country or even globally.
- Reduced stress and burnout: Remote work can reduce stress and burnout by eliminating the need to navigate heavy traffic, deal with office politics, or work in high-stress environments.
Requirements for Remote Utilization Review Nurse Jobs
To be eligible for remote utilization review nurse jobs, candidates typically need to meet the following requirements:
- Registered Nurse (RN) license: A current RN license is required for most utilization review nurse positions.
- Utilization review certification: Many employers require or prefer candidates with utilization review certification, such as the Certified Utilization Review Nurse (CURN) or the Certified Professional in Healthcare Management (CPHM) credentials.
- Experience in utilization review: Most employers require candidates to have experience in utilization review, case management, or a related field.
- Strong analytical and communication skills: Utilization review nurses need to be able to analyze complex data, communicate effectively with stakeholders, and make sound decisions.
Education and Training
While a bachelor's degree in nursing is often preferred, some employers may accept candidates with an associate's degree in nursing or a related field. Utilization review nurses typically need to complete ongoing education and training to stay current with changing healthcare regulations, technologies, and best practices.
Job Opportunities and Salary Ranges
Remote utilization review nurse jobs are available in various settings, including:
- Health insurance companies: Many health insurance companies hire utilization review nurses to review medical claims and determine coverage.
- Healthcare providers: Hospitals, health systems, and medical groups often employ utilization review nurses to optimize patient care and reduce costs.
- Telehealth companies: With the growth of telehealth, companies are hiring utilization review nurses to review medical records and provide virtual care coordination.
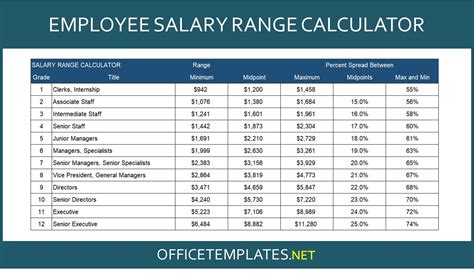
Salary ranges for remote utilization review nurse jobs vary depending on factors such as location, experience, and employer. However, here are some approximate salary ranges:
- Entry-level positions: $60,000 - $80,000 per year
- Mid-level positions: $80,000 - $110,000 per year
- Senior-level positions: $110,000 - $140,000 per year
Conclusion
Remote utilization review nurse jobs offer a unique opportunity for nurses to work in a dynamic and growing field. With the increasing demand for cost-effective and high-quality patient care, utilization review nurses play a critical role in shaping the future of healthcare. By understanding the benefits, requirements, and job opportunities available in this field, nurses can take the first step towards a rewarding and challenging career in remote utilization review nursing.
We invite you to share your thoughts and experiences with remote utilization review nurse jobs in the comments section below. If you have any questions or would like to learn more about this topic, please don't hesitate to ask.
What is the primary goal of utilization review nursing?
+The primary goal of utilization review nursing is to optimize patient outcomes while minimizing unnecessary healthcare expenditures.
What are the typical salary ranges for remote utilization review nurse jobs?
+Salary ranges for remote utilization review nurse jobs vary depending on factors such as location, experience, and employer. However, approximate salary ranges are: entry-level positions ($60,000 - $80,000 per year), mid-level positions ($80,000 - $110,000 per year), and senior-level positions ($110,000 - $140,000 per year).
What certifications are required or preferred for utilization review nurse positions?
+Many employers require or prefer candidates with utilization review certification, such as the Certified Utilization Review Nurse (CURN) or the Certified Professional in Healthcare Management (CPHM) credentials.
